As women navigate the journey of life, menopause marks a significant transition. It’s a time of physical, emotional, and cognitive changes that can impact overall well-being. Understanding the signs of onset of menopause can empower women to prepare for and manage this natural phase with knowledge and confidence.
Menopause is characterized by a decline in estrogen production, which triggers a cascade of changes in the body. While every woman’s experience is unique, recognizing the common signs can help women anticipate and address the challenges they may face.
Physical Symptoms
The onset of menopause marks a significant hormonal shift in a woman’s life, accompanied by various physical symptoms. These changes are primarily caused by declining levels of estrogen and progesterone, hormones that play crucial roles in regulating the menstrual cycle and maintaining reproductive health.
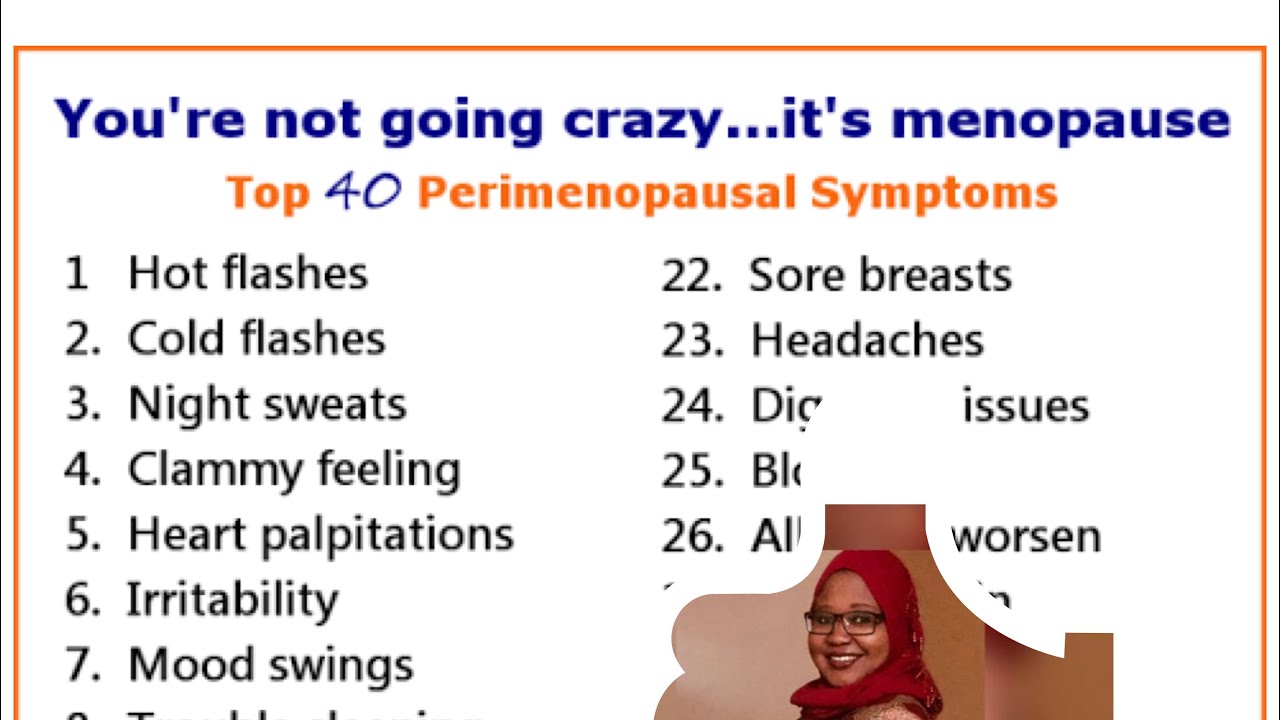
Understanding the physical signs of menopause can help women prepare for and manage the transition. Here’s a comprehensive list of common symptoms, their underlying causes, and their potential impact on overall health and well-being:
Hot Flashes and Night Sweats
- Hot flashes are sudden feelings of intense heat that spread over the face, neck, and chest, often accompanied by sweating.
- They occur due to changes in the hypothalamus, the part of the brain that regulates body temperature.
- Hot flashes can disrupt sleep, increase irritability, and affect mood.
Irregular Periods
- Menopause typically begins with irregular periods, which can become more frequent or less frequent, with varying flow.
- This irregularity is caused by fluctuating hormone levels, which affect the menstrual cycle.
- Irregular periods can make it difficult to predict ovulation and plan for pregnancy.
Vaginal Dryness
- Declining estrogen levels can lead to thinning and dryness of the vaginal walls, resulting in discomfort during intercourse.
- Vaginal dryness can also increase the risk of urinary tract infections (UTIs) and other vaginal infections.
- It can impact sexual health and overall well-being.
Mood Changes
- Hormonal fluctuations during menopause can affect mood, leading to irritability, anxiety, or depression.
- These changes are influenced by the interaction between hormones and neurotransmitters in the brain.
- Mood swings can impact personal relationships, work performance, and overall quality of life.
Sleep Disturbances
- Night sweats, hot flashes, and hormonal changes can disrupt sleep patterns.
- Insufficient sleep can lead to fatigue, difficulty concentrating, and impaired daytime functioning.
- Sleep disturbances can significantly affect overall health and well-being.
Osteoporosis
- Estrogen plays a crucial role in maintaining bone density.
- As estrogen levels decline during menopause, bone loss accelerates, increasing the risk of osteoporosis, a condition characterized by weakened and brittle bones.
- Osteoporosis can lead to fractures and other bone-related health issues.
Heart Disease
- Estrogen has protective effects on the heart and blood vessels.
- With declining estrogen levels, women may become more susceptible to heart disease, including coronary artery disease and stroke.
- Maintaining a healthy lifestyle, including regular exercise and a balanced diet, is crucial for reducing the risk of heart disease during menopause.
Weight Gain
- Hormonal changes during menopause can lead to increased body fat, particularly around the abdomen.
- Declining estrogen levels can affect metabolism and appetite regulation.
- Weight gain can contribute to other health issues, such as heart disease and type 2 diabetes.
Emotional Changes
Menopause brings about a multitude of emotional shifts that can be both challenging and empowering. These changes stem from the hormonal fluctuations that occur as estrogen and progesterone levels decline.
Mood Swings and Irritability
Estrogen has a calming effect on the brain, so its decline can lead to mood swings, irritability, and anxiety. These symptoms can be exacerbated by other factors such as stress, sleep disturbances, and hormonal imbalances.
Emotional Sensitivity
Progesterone is responsible for regulating emotional responses. Its decline during menopause can make individuals more sensitive to emotional triggers, resulting in heightened feelings of sadness, anger, or overwhelm.
Coping Strategies
Coping with the emotional challenges of menopause involves self-care, emotional regulation techniques, and seeking professional support when needed.
- Engage in regular exercise, which releases endorphins that have mood-boosting effects.
- Practice relaxation techniques such as deep breathing, yoga, or meditation to reduce stress and anxiety.
- Get adequate sleep, as sleep deprivation can exacerbate emotional instability.
- Connect with others and share your experiences with friends, family, or support groups.
- Consider therapy or counseling if emotional symptoms become overwhelming or interfere with daily life.
Cognitive Function
Menopause can affect cognitive function in several ways. Some women may experience a decline in cognitive abilities, such as memory, attention, and executive function. Others may find that their cognitive function remains stable or even improves during this transition.
Research Evidence
Research on the effects of menopause on cognitive function has yielded mixed results. Some studies have found that women in menopause are more likely to experience cognitive decline than women who have not yet reached menopause. Other studies have found no significant differences in cognitive function between menopausal and non-menopausal women.
- A study published in the journal “Menopause” found that women in menopause were more likely to have difficulty with memory and attention than women who were not in menopause.
- A study published in the journal “Neurology” found that women who had experienced surgical menopause were more likely to develop dementia than women who had not experienced surgical menopause.
- A study published in the journal “The Journal of the North American Menopause Society” found that women who were taking hormone therapy were less likely to experience cognitive decline than women who were not taking hormone therapy.
Sleep Disturbances
During menopause, many women experience significant changes in their sleep patterns. These disturbances can be caused by hormonal fluctuations, as well as other factors such as stress, anxiety, and hot flashes.
The most common sleep problems experienced by women during menopause include:
- Insomnia: Difficulty falling or staying asleep
- Early morning awakening: Waking up several hours before the desired time and being unable to fall back asleep
- Non-restorative sleep: Feeling unrested or tired after a full night’s sleep
These sleep disturbances can have a significant impact on a woman’s overall health and well-being. They can lead to fatigue, irritability, difficulty concentrating, and decreased productivity.
There are a number of things that women can do to improve their sleep quality during menopause:
- Establish a regular sleep schedule and stick to it as much as possible, even on weekends.
- Create a relaxing bedtime routine that may include taking a warm bath, reading a book, or listening to calming music.
- Make sure your bedroom is dark, quiet, and cool.
- Avoid caffeine and alcohol before bed.
- Get regular exercise, but avoid exercising too close to bedtime.
- If you can’t fall asleep after 20 minutes, get out of bed and do something relaxing until you feel tired.
If you are experiencing significant sleep disturbances during menopause, talk to your doctor. There may be an underlying medical condition that is contributing to your sleep problems.
Cardiovascular Health

Menopause can have a significant impact on cardiovascular health. The decline in estrogen levels during this time can lead to changes in blood pressure, cholesterol levels, and the structure and function of blood vessels.
These changes can increase the risk of developing cardiovascular diseases such as heart disease, stroke, and heart failure.
Risk Factors
Several factors can contribute to the increased risk of cardiovascular disease during and after menopause, including:
- Decreased estrogen levels:Estrogen has a protective effect on the heart and blood vessels. Its decline during menopause can lead to increased inflammation, oxidative stress, and plaque buildup in the arteries.
- Increased blood pressure:Menopause can cause an increase in blood pressure, which is a major risk factor for cardiovascular disease.
- Changes in cholesterol levels:Menopause can lead to an increase in LDL (bad) cholesterol and a decrease in HDL (good) cholesterol, which can increase the risk of plaque buildup in the arteries.
- Changes in blood vessel structure and function:Menopause can cause changes in the structure and function of blood vessels, making them less flexible and more prone to plaque buildup.
Recommendations
There are several things women can do to maintain cardiovascular health during and after menopause, including:
- Maintain a healthy weight:Obesity is a major risk factor for cardiovascular disease. Maintaining a healthy weight can help reduce the risk of developing cardiovascular problems.
- Exercise regularly:Exercise helps to improve cardiovascular health by strengthening the heart and blood vessels, reducing blood pressure, and improving cholesterol levels.
- Eat a healthy diet:A healthy diet that is low in saturated fat, cholesterol, and sodium can help reduce the risk of cardiovascular disease.
- Quit smoking:Smoking is a major risk factor for cardiovascular disease. Quitting smoking can significantly reduce the risk of developing cardiovascular problems.
- Manage blood pressure:High blood pressure is a major risk factor for cardiovascular disease. If you have high blood pressure, it is important to take medication to lower it.
- Manage cholesterol levels:High cholesterol levels are a major risk factor for cardiovascular disease. If you have high cholesterol, it is important to take medication to lower it.
- Get regular checkups:Regular checkups can help identify and manage risk factors for cardiovascular disease. Talk to your doctor about your risk factors and what you can do to reduce them.
Bone Health
Menopause marks a significant transition for women, and one of its most notable impacts is on bone health. The hormonal changes that occur during this time can lead to an increased risk of osteoporosis, a condition characterized by weakened and brittle bones that are more susceptible to fractures.
The primary culprit behind this increased risk is the decline in estrogen production. Estrogen plays a crucial role in regulating bone metabolism, promoting the formation of new bone and inhibiting its breakdown. As estrogen levels drop during menopause, this delicate balance is disrupted, leading to a net loss of bone.
Other Contributing Factors
- Age:Bone density naturally decreases with age, regardless of menopause.
- Calcium and Vitamin D deficiency:These nutrients are essential for bone health.
- Certain medications:Some medications, such as corticosteroids, can interfere with bone metabolism.
- Lifestyle factors:Smoking, excessive alcohol consumption, and physical inactivity can all contribute to bone loss.
Recommendations for Maintaining Bone Health
Fortunately, there are several measures women can take to maintain bone health and prevent osteoporosis during and after menopause:
- Calcium and Vitamin D:Ensure adequate intake through diet and supplements if necessary.
- Weight-bearing exercise:Regular exercise, such as walking, running, and dancing, helps build bone density.
- Avoid smoking and excessive alcohol:These habits can harm bone health.
- Consider hormone replacement therapy (HRT):HRT can help preserve bone density, but it’s important to discuss the risks and benefits with a healthcare professional.
- Bone density screening:Regular screenings can help identify bone loss early and guide appropriate interventions.
Lifestyle Modifications
Menopause can significantly impact a woman’s overall health and well-being. Implementing positive lifestyle modifications during this transition can effectively manage menopausal symptoms and enhance overall health.Adopting a healthy diet, engaging in regular exercise, practicing stress management techniques, and maintaining other healthy habits are crucial during menopause.
These changes can alleviate symptoms, reduce the risk of chronic diseases, and promote overall well-being.
Dietary Modifications
A balanced diet rich in fruits, vegetables, and whole grains is essential during menopause. Maintaining a healthy weight can reduce the severity of hot flashes and night sweats. Consuming calcium-rich foods, such as dairy products and leafy green vegetables, is crucial for bone health.
Limiting caffeine and alcohol intake can also help manage symptoms.
Exercise
Regular exercise is vital for overall health and can alleviate menopausal symptoms. Aerobic activities, such as walking, swimming, or cycling, can reduce hot flashes and improve mood. Weight-bearing exercises, such as strength training or dancing, help maintain bone density and reduce the risk of osteoporosis.
Stress Management
Stress can exacerbate menopausal symptoms. Engaging in stress-reducing activities, such as yoga, meditation, or spending time in nature, can help manage stress levels and improve overall well-being.
Other Healthy Habits
Getting enough sleep, avoiding smoking, and limiting alcohol consumption are additional healthy habits that can support overall health during menopause. Regular check-ups with a healthcare provider can help monitor health and ensure appropriate care.By implementing these lifestyle modifications, women can effectively manage menopausal symptoms, improve their overall health, and enhance their well-being during this transition.
Medical Interventions
Menopause can bring about a wide range of symptoms that can significantly impact a woman’s quality of life. Medical interventions offer a variety of options to manage these symptoms and improve overall well-being during this transition.
The most common medical intervention for menopausal symptoms is hormone replacement therapy (HRT). HRT involves taking hormones, such as estrogen and progesterone, to replace the hormones that the body stops producing during menopause. HRT can effectively relieve hot flashes, night sweats, vaginal dryness, and other symptoms.
Benefits of HRT
- Reduces hot flashes and night sweats
- Improves vaginal dryness
- Protects against bone loss
- May reduce the risk of heart disease
Risks of HRT
- Increased risk of blood clots
- Increased risk of breast cancer
- Increased risk of endometrial cancer
- May cause nausea, bloating, and breast tenderness
Antidepressants can also be used to treat menopausal symptoms, particularly hot flashes and night sweats. They work by increasing the levels of serotonin and norepinephrine in the brain, which can help regulate body temperature and mood.
Benefits of Antidepressants
- Reduces hot flashes and night sweats
- Improves mood
- Reduces anxiety
Risks of Antidepressants
- May cause nausea, dizziness, and dry mouth
- May interact with other medications
- May not be suitable for women with a history of depression or bipolar disorder
Other medications, such as gabapentin and clonidine, can also be used to treat specific menopausal symptoms. Gabapentin can help reduce hot flashes, while clonidine can help reduce blood pressure and anxiety.
It is important to discuss the benefits and risks of all medical interventions with a healthcare provider before starting treatment. The best treatment plan will depend on a woman’s individual symptoms, medical history, and preferences.
If menopausal symptoms are severe or interfere with daily life, it is important to seek medical advice. A healthcare provider can help determine the best course of treatment and provide support during this transition.
Cultural and Social Aspects

The experience of menopause is not only influenced by biological factors but also by cultural and social factors. Cultural norms, beliefs, and practices shape how women perceive and manage menopausal symptoms.
In some cultures, menopause is seen as a natural transition and a time of wisdom and respect. In others, it is viewed as a time of decline and loss. These cultural beliefs can impact women’s self-perception and their willingness to seek help for menopausal symptoms.
Social Support
Social support plays a vital role in supporting women during menopause. Family, friends, and community members can provide emotional and practical assistance, helping women cope with symptoms and navigate the challenges of this transition.
- Emotional support can include listening to concerns, providing reassurance, and offering encouragement.
- Practical support may involve assisting with childcare, transportation, or meal preparation.
Community Resources
Community resources can also provide valuable support for women during menopause. These resources may include:
- Menopause support groups
- Educational programs
- Counseling services
These resources can provide women with information, support, and a sense of community, helping them navigate the challenges of menopause.
Helpful Answers
What are the most common physical signs of menopause?
Hot flashes, night sweats, vaginal dryness, irregular periods, and sleep disturbances are among the most prevalent physical signs.
How do emotional changes manifest during menopause?
Mood swings, irritability, anxiety, and depression are common emotional experiences associated with the hormonal fluctuations of menopause.
Can menopause affect cognitive function?
Some women may experience cognitive changes, such as memory lapses, difficulty concentrating, and reduced verbal fluency, during menopause.